Heroin-assisted treatment (HAT) refers to the prescription of pharmaceutical heroin (diacetylmorphine) to people with severe opioid use disorders who have not responded well to more traditional forms of treatment like methadone or buprenorphine.
Typically, clients are provided injectable or inhalable heroin 2-3 times per day by prescription, and they consume it on-site in a medically-supervised clinic setting. Some of these programs also provide access to hydromorphone as an option to patients. In clinical research trials, participants preferred diacetylmorphine or hydromorphone equally.
HAT provides legal access to pharmaceutical heroin to prevent patients from buying it on the illicit market where it may be adulterated, or mixed, with unknown drugs or substances. Patients are given access to harm reduction interventions, connections with substance use disorder treatment and medical services, and social supports such as housing assistance.
Over a decade of research of existing programs has established the positive impacts of HAT, including:
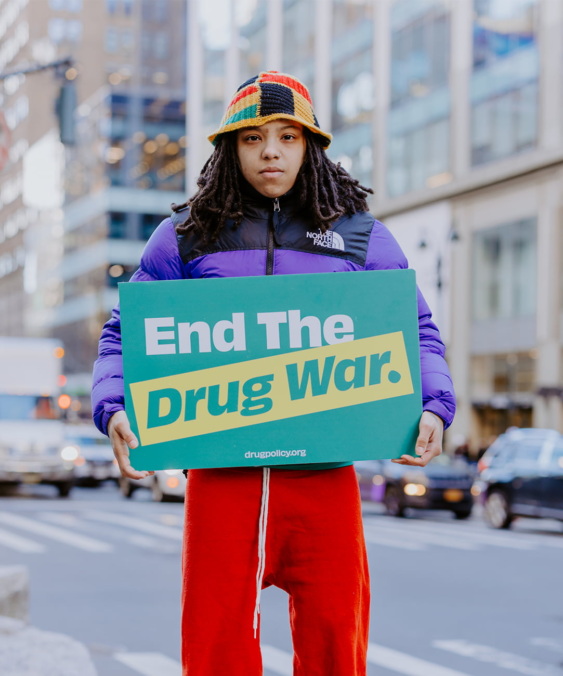
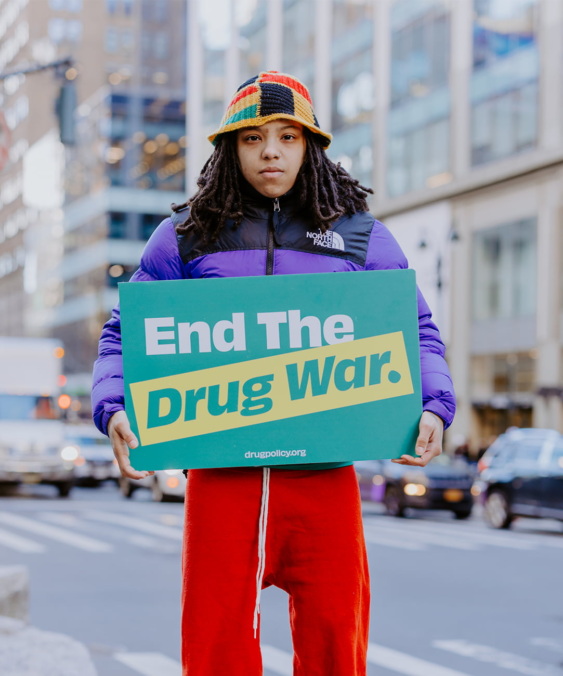
No HAT programs exist in the U.S. due to a host of political and ideological barriers, including:
There can be a lack of community support based on fears that HAT will cause an increase in drug use and crime. These fears are unfounded. In areas surrounding existing HAT sites, there has been no evidence of increased community drug use, initiation of injection drug use, or drug-related crime.
Notifications