Shayna Samuels at 718-541-4785 or Ariel Kalishman at 212-613-8036
Trenton–A report released today by the firm New Jersey Economics claims that New Jersey taxpayers could save millions of dollars in medical costs by allowing injection drug users access to clean needles to prevent the spread of HIV, hepatitis C, and other blood-borne diseases.
In New Jersey, the sharing of contaminated syringes by injection drug users is the leading cause of HIV and hepatitis C infections. While nationally about 25% of HIV infections are related to injection drug use, in New Jersey 46% of infections are related to sharing contaminated needles. New Jersey is almost alone among states in allowing no access whatsoever to clean syringes; and is one of only five states that currently bans the sale of sterile syringes to adults without a prescription. Even in states that require a prescription to purchase a syringe, such as California and Pennsylvania, there are state- or municipally-mandated syringe exchange programs.
Donald M. Scarry, principal economist with New Jersey Economics, who researched and wrote the report, said, “There are significant unintended consequences from New Jersey’s restrictive regulations on the sale and possession of syringes; namely, a public health crisis and the financial costs that go with it.”
New Jersey has the 5th highest adult HIV rate, the 3rd highest pediatric AIDS rate, and the highest percentage of women infected with HIV in the nation. The new report found that around the country and the world, decreased HIV infection rates occur as a result of allowing for increased access to sterile syringes. The report estimates that lifetime AIDS care costs approximately $227,000, and that if new HIV infection rates continue at present levels, New Jersey could expect public health costs to increase by $400 million annually. In contrast, a clean needle costs ten cents.
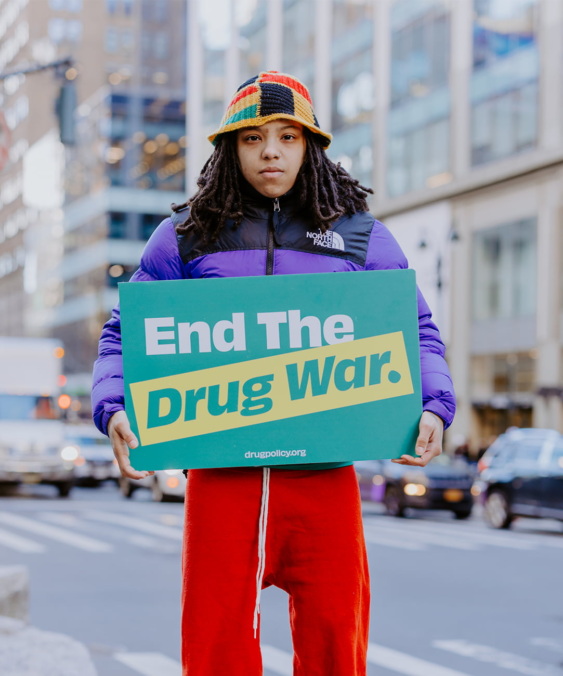
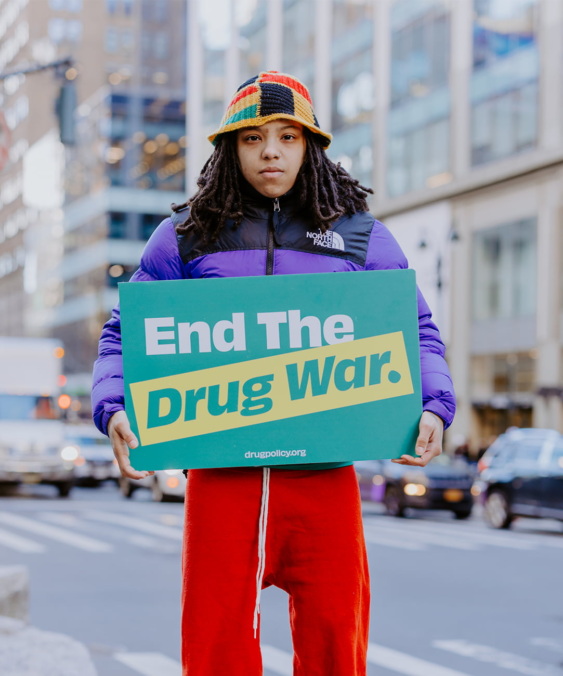
The new report is expected to add to the growing support for Assembly Bill 3645, which would allow for increased access to sterile syringes to prevent the spread of HIV, hepatitis C, and other blood-borne diseases. The legislation would allow for the sale of syringes in pharmacies without a prescription, and allow municipalities and public health providers to incorporate syringe exchange services into their HIV prevention programs. Recently the Camden, Jersey City, and Newark city councils unanimously passed resolutions supporting the legislation, and a coalition of organizations including the Medical Society of New Jersey, the New Jersey State Nurses Association, several pharmacy groups, the Black Minister Council, the Drug Policy Alliance, and Hyacinth AIDS Foundation have formed a coalition called the Campaign for a Healthier New Jersey, to support the legislation.
Roseanne Scotti, Director of the New Jersey Drug Policy Project-Drug Policy Alliance, which commissioned the study, said: “There have been many studies looking at the costs and benefits of sterile syringe access and they have all concluded that increased access to sterile syringes reduces the spread of injection-related diseases, does not increase drug use, and saves taxpayers money in avoidable medical costs. At a time when New Jersey is facing the biggest budget shortfall in history, it makes no sense to continue a restrictive syringe access policy that most states abandoned long ago.”
“This is an opportune time to look at both the public health and economic priorities to prevent HIV and leverage more funds for appropriate care,” said Riki Jacobs, Executive Director of the Hyacinth AIDS Foundation. “It is clear that syringe access makes economic sense and saves lives.”
“Study after study has shown that increasing access to syringes has stemmed the spread of HIV/AIDS, yet there is still a negative stigma associated with such programs,” said Assemblyman Reed Gusciora (D. Mercer) sponsor of A3645. “Once people are educated as to the benefits of such programs, they will see that these ideas not only make sense socially, but also economically.”
Download Access to Sterile Syringes and Public Health Costs in New Jersey: Suggestions for Public Policy
Notifications